With Histotripsy, ‘The Journey is Not Over’
By Wendy Sutton

“I’m fortunate to be here two years and a month after expecting to survive only 90 days, thanks to the University of Michigan and their team. Histotripsy has vast potential. Anything learned from this benefits others, and there’s still life I want to live. As long as I can maintain my quality of life, I’m pushing forward. The journey isn’t over.”


Tom Ryan was in good health, enjoying retirement and travel with his wife when he began experiencing lower back pain he thought was muscle soreness.
In March 2023, a CT scan revealed a much more serious issue – a pancreatic tumor.
Referred to the University of Michigan Rogel Cancer Center’s Multidisciplinary Pancreatic Cancer Program, he began intensive treatment involving chemotherapy, an experimental AstraZeneca drug and a Whipple surgery, which removes parts of the pancreas, small intestine, gallbladder and bile duct. After a year of treatment, Ryan’s scans were tumor-free.
“It was a big surprise to everyone,” he recalled. “It seemed likely I would be cancer free, which was really momentous because that just doesn’t happen.”
In September 2024, however, a follow-up CT scan showed new liver tumors and a suspicious area near his pancreas. Ryan resumed chemotherapy, along with a drug that proved ineffective, prompting him and his doctor to seek new trial therapies. During his research, he came across an article about histotripsy, a new ablation technology developed at the University of Michigan.
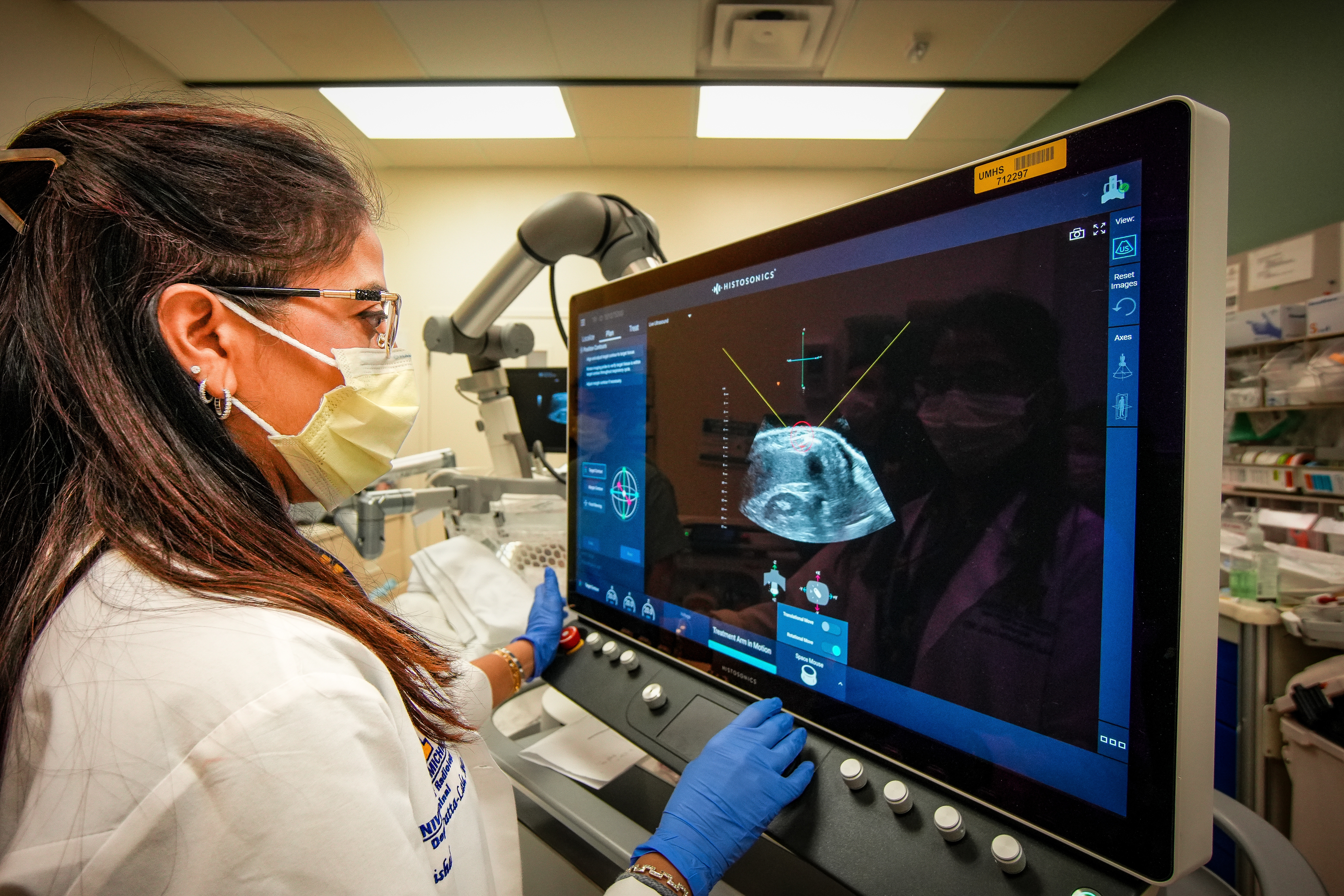
Histotripsy, developed through research led by Dr. Zhen Xu, a professor of biomedical engineering at U-M, uses ultrasound to create microbubbles from naturally occurring gas pockets within targeted tissue. This noninvasive process breaks down cancerous tissue at the cellular level with minimal damage to surrounding healthy tissue.
“I got really excited about the prospect,” he said. “I asked my doctor about it early on, but he felt the timing wasn’t right because the tumors were advancing. But each time we talked, I brought it up. When the latest scan showed that the chemo was shrinking the tumors, he agreed it was time to make the referral.”
Days later, Ryan received a call from the office of Dr. Mishal Mendiratta-Lala, Agree Family Research Professor of Image Guided Intervention and clinical professor of radiology at U-M, to arrange a screening ultrasound. He soon traveled to Ann Arbor for his histotripsy procedure.
“It’s probably the most benign form of therapy, meaning the least amount of discomfort, that you could imagine having,” Ryan said. “All other forms of therapy come with significant potential side effects and drawbacks, but histotripsy does not. If I ever get another tumor they can access, I would do it again.”
Histotripsy is still in its early stages, with ongoing research aimed at improving and expanding its applications. Federal research funding is crucial to these efforts.
Ryan said he feels grateful for the opportunity to help tell the story of this remarkable technology.
“I’m fortunate to be here two years and a month after expecting to survive only 90 days, thanks to the University of Michigan and their team,” he said. “Histotripsy has vast potential. Anything learned from this benefits others, and there’s still life I want to live. As long as I can maintain my quality of life, I’m pushing forward. The journey isn’t over.”
