The Future, Fast: Emergency Medicine at U-M Positions AI as a Department-Wide Strategy
By Danielle Jimenez, Communication Specialist, Department of Emergency Medicine, Michigan Medicine
Artificial intelligence is transforming medicine nationwide — and at the University of Michigan, the Department of Emergency Medicine is moving faster and thinking bigger.
Rather than using AI as a one-off tool, the department is adopting it as a core strategy — reshaping everything from education and clinical decision-making to operations, discovery and diagnostics. It’s a vision that places emergency medicine at the forefront of AI’s role in redefining academic medicine.
“We’re not just experimenting with AI,” said Dr. Prashant Mahajan, William G. Barson Collegiate Professor and chair of the department of emergency medicine. “We are adopting it as a strategy. We are integrating it across everything we do.”
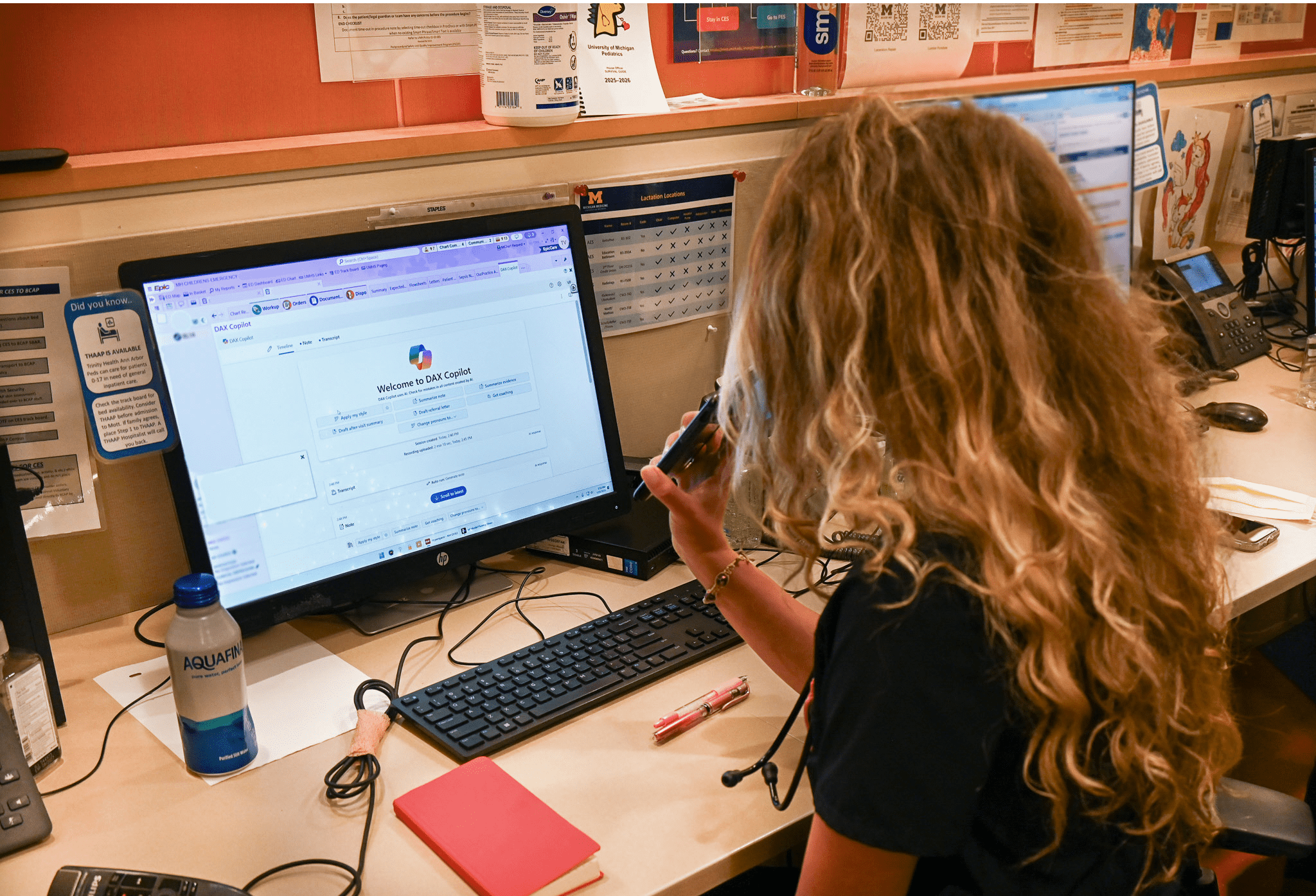

Teodora Vercerdi, PA-C at Michigan Medicine, uses DAX Copilot at her workstation in the Pediatric Emergency Department at C.S. Mott Children’s Hospital to streamline documentation during a busy shift in the Emergency Department. Powered by AI, DAX listens to patient encounters and automatically drafts clinical notes, helping clinicians save time, reduce burnout, and stay more focused on patient care. It’s one of several AI tools being explored to improve efficiency and outcomes in emergency medicine.
Why Emergency Medicine?
With more than 140 million emergency visits annually in the U.S., the emergency department, or ED, is the front door to the health care system — where decisions happen in seconds, and mistakes can be deadly. That high-stakes environment makes emergency medicine a natural proving ground for AI.
“In emergency medicine, every interaction between a patient and a provider has a diagnostic element,” said. Mahajan, also a professor of pediatrics and emergency medicine.
The ED often operates in a state of controlled chaos, where multiple evolving cases are assessed simultaneously by providers with diverse training and backgrounds. The cognitive and physical demands on providers are immense.
Nationwide, EDs face a growing crisis of overcrowding, driven by more frequent and more complex patient cases. Many of these complex conditions require extended hospital stays, and hospitals are struggling to discharge patients due to a shortage of outpatient options like skilled nursing facilities.
“It is imperative that we enhance diagnostic excellence to ensure safe care and better outcomes,” Mahajan said. “We must also support provider wellbeing — burnout in emergency medicine is nearing 60%. Still, more than 90% of diagnostic decisions lead to life-saving interventions and positive outcomes.”
At Michigan Medicine, the ED team is thinking bigger and aiming higher. AI can accelerate real-time diagnostic decisions, reduce patient harm and ease the burden on providers.
“AI should be more than a tool; it should be a strategy for transforming emergency care,” Mahajan said. “Every patient interaction in the ED involves an element of diagnosis, and decisions must be made quickly, with little margin for error.”
By adopting AI as a department-wide strategy, Michigan Medicine is asking: Can it improve clinician training? Reduce diagnostic error? Support real-time decisions? Prevent burnout? And do it all safely, ethically and equitably?
Chair’s Initiative: Embedding AI Across Emergency Care
To drive this transformation, Dr. Mahajan launched the “Chair’s Initiative: AI in Emergency Care” – a departmentwide effort spanning four academic domains: education, clinical care, research and advocacy, all with a focus on safe, transparent and ethical implementation. AI is being integrated into both existing workflows and new innovations across all domains.
The initiative includes a series of pragmatic interventions. Teams will rapidly prototype tools to detect critical illnesses earlier and evaluate AI-driven decision aids designed to expedite diagnoses for conditions like pulmonary embolism and sepsis.
In the education domain, teams will explore how AI can enhance clinical training, including the impact of brief, just-in-time learning interventions.
In research, the department will lead robust trials comparing AI-enabled tools with traditional decision aids. It will also advocate for safe, ethical and patient-centered technologies across the field.
By embedding AI across education, clinical care and research, the department aims to reduce diagnostic errors, empower clinicians and improve access to timely, high-quality care, laying the groundwork for national leadership in diagnostic excellence.
Pushing the Boundaries of Possibility
Faculty are already piloting AI-driven projects that address real-world challenges in emergency care.
Mahajan, along with Douglas Craig, statistician staff specialist, and Dr. Ruta Sharangpani, research department specialist, is using large language models to analyze over a million ED notes to predict visit necessity and uncover patterns clinicians may overlook. Craig is also developing Clara Bedside Assistant, a palm-sized, voice-activated assistant that provides secure, real-time clinical guidance without an internet connection.
Tools like PICTURE, developed at the Max Harry Weil Institute for Critical Care Research and Innovation, help predict patient deterioration up to 30 hours in advance and are already in use. AHI, another AI system, detects blood flow instability from ECG data, offering up to 26 hours of lead time before symptoms. Both are changing how teams intervene before critical events occur.
Dr. Alex Janke, clinical assistant professor of emergency medicine, is developing feedback tools to help physicians learn from their own diagnostic patterns, improving performance over time.
Dr. Max Spadafore, director of educational informatics for the Office of Medical Student Education and clinical assistant professor of emergency medicine, is exploring how ambient AI documentation might influence clinical reasoning in medical students, and whether it risks dulling their ability to think like a doctor. He’s also building algorithms that coach faculty on how to write more effective feedback.
Others are using generative AI to automate literature reviews, draft grants and simulate trial designs.
“There’s a misconception that large language models are just chatbots,” Mahajan said. “But they’re capable of enhancing real-time decisions, documentation, research and even communication.”
The End Goal: Diagnostic Excellence
At the heart of the initiative is a commitment to what Mahajan calls “diagnostic excellence.” That means reducing errors, empowering clinicians and improving care.
“Every patient deserves an accurate and timely diagnosis,” Mahajan said. “By reducing cognitive load and giving our providers better tools, we can move patients through the system faster, improve safety and reduce burnout. That’s the real promise of AI.”
The stakes are high. About 5% of ED patients experience a diagnostic error, equating to 7.5 million missed or delayed diagnoses and more than $1 trillion in annual impact.The department believes that AI, if used carefully, can help close that gap.
Mahajan stresses that success depends on doing it right.
“We need to make sure the algorithms are accurate, reliable and safe,” he said. “And we need to study their impact. Does it improve care?”
AI as Culture, Not Just Code
For Michigan Medicine’s Department of Emergency Medicine, this is just the beginning. By embedding AI into the department’s culture, leaders aim to set a new standard for the future of academic medicine.
“AI is no longer just a product of our research,” Mahajan said. “It is a strategy. It is a goal. And we want everyone – clinicians, educators, researchers – to see it as a future they’re building toward.”
